
The provision of health services in both rural and urban communities is complex and composed of many pieces. One particular part of the rural health care mix that has gathered significant attention in both the popular press and academic literature (e.g., Kaufman, et.al. 2016; Kissi, Walston, and Badar 2021) is the alarming rate of rural hospital closures. Headlines such as CNN’s July 31, 2021 story entitled “[h]ow the pandemic killed a record number of rural hospitals” or Becker’s Hospital Review February 18, 2022 story entitled “[s]taffing crisis, payment cuts put 453 hospitals at risk of closure” are increasingly common. In addition, the national shortage of nurses, particularly in rural America, has also garnered significant attention (e.g., Scheidt, Heyen and Greever-Rice 2021; Advnski and Morgan 2021). But one important piece of the rural and urban, health care delivery system that received little attention are community pharmacies. Analysis of rural pharmacies in the U.S. by Salako, Ullrich and Mueller (2018) found that between 2003 and 2018, 1,231 independently owned rural pharmacies (16.1 percent) in the United States have closed, with the most drastic decline occurring between 2007 and 2009. This is largely due to the implementation of Medicare Part D reimbursement that made the process less cost effective for independent pharmacies (Klepser, Xu, Ullrich, and Mueller 2011). In a complementary analysis Qato and her coauthors (2017) found that many more rural and poorer communities did not have access to any pharmacy services. More importantly, they found that many independent pharmacies are being replaced with chain or franchise pharmacies that reduce the level of services offered to customers. For example, Qato and coauthors found that less than one percent of “mass retail” pharmacies offered home delivery of prescriptions whereas 67 percent of independent pharmacies offered such a service.Pharmacies are an overlooked and underappreciated resource for health care, particularly in rural areas (Straub and Straub 1999). Pharmacists play a crucial role on apatient’s health care team by ensuring medications are safe for patients, providing patient counseling, and being an easily accessible source for information and care. As noted by Stratton (2001) pharmacists often play a prominent role as a provider of first-contact care in rural communities. Furthermore, pharmacies provide preventative health services such as immunizations, blood pressure checks and glucose monitoring. Providing these routine services can help prevent patients from needing more costly care such as hospital stays. Particularly in rural areas, where patients have less access to health care services, pharmacies play a vital role in the delivery of health care. Casey, Klingner, and Moscovice (2002) note that limited access to pharmacy services may cause rural consumers to delay or forego essential treatment with prescription medications thus exacerbating underlying health problems.
In rural areas, pharmacies may be the only source of qualified health care services, especially as rural hospitals close or consolidate. Pharmacists can counsel, monitor, and advise patients on their conditions in a setting that is more convenient (and affordable) than a clinical setting. Patients have also indicated that they are often more comfortable asking the pharmacist questions than they are their doctor. As discussed in more detail below, pharmacies in rural areas are much more likely to be independently owned, hence the decline in independent pharmacies will disproportionately impact rural areas that are already lacking access to healthcare services overall compared to more urban settings. This will lead to a loss of not only medication access, but to health care access:
“If pharmacies are closed, especially in places where there’s no other health care provider, then you’ve got essentially a health care desert…” Michael Hogue, President of the American Pharmacists Association (Hawryluk, 2021 (on-line no page number)).
Especially for underserved locations, the option of having prescriptions delivered through the mail may seem like an attractive option when a community pharmacy is unavailable. The push to increase prescriptions-by-mail services (or on-line services) may be convenient for routine medications, but patients with ailments requiring more immediate relief may not want to wait several days for prescriptions to be delivered. Those that do not have access to a local community retail pharmacy may have to drive to a more urban area for prescription services. In addition, transportation in rural areas is often a barrier to services, especially for those who are elderly and/or disabled, and these groups use more prescription medications than others (Pednekar and Peterson 2018). Having a pharmacy in the community benefits everyone needing access to prescriptions, medication counseling and oversight. Further analysis is needed of the effects of transportation and access to pharmacies, particularly in rural areas.For many smaller rural communities, locally owned independent pharmacies are the anchors for downtowns and is often a major draw for people to travel into the downtown. In addition to prescriptions, over-the-counter medicines, and direct health care services, many of these pharmacies could be thought of as a convenience store that offers a wide range of retail items. The rash of closures of rural independent pharmacies identified by Salako, Ullrich, and Mueller (2018) has eliminated many anchor businesses and created vacant storefronts in many rural communities. The pressure that these rural independent pharmacies face impacts not only the range of health care services for rural residents but also the vibrancies of many rural downtowns.
To explore the trends in community pharmacies over time and across the rural-urban spectrum we use data from the Business Dynamics Research Consortium, a project of the University of Wisconsin, Institute for Business and Entrepreneurship. These data are from a verified version of Data Axle Business Historical databases with establishment data from 1997 through the current year. In this sense, our core data differs from Salako, Ullrich, and Mueller (2018) who use the data files provided by the National Council for Prescription Drug Programs (NCPDP).
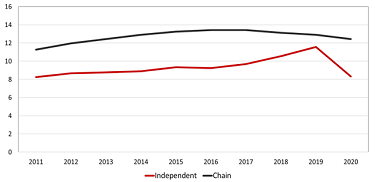
Between 2011 and 2020 the average number of chain pharmacies in a given U.S. county increased from 11.2 in 2011 to 13.4 in both 2017 and 2018, but then declined to 12.4 by 2020 but the number of independent pharmacies went from 8.2 in 2011 to a peak of 11.5 in 2019, then plummeted to 8.3 in 2020 (Figure 1). This latter drop is likely due to the impact of COVID-19 but is unclear from these data. There are three general observations: (1) the average number of chain retail pharmacies is greater than independents, (2) there is a modest upward trend in both chain and independent retail pharmacies (although the upward trend for chain pharmacies appears to have stalled and reversed itself after 2018), and if COVID-19 has impacted pharmacies it is impacting independent pharmacies the greatest. This latter result makes intuitive sense in that chain pharmacies have the advantage of scale to ride out short-term economic shocks. Independent pharmacies, much like any other independent business, do not have the comparable resources to weather economic shocks, particularly sustained longer-term shocks.
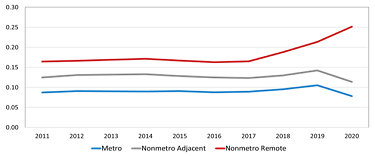
To look across the rural-urban spectrum we use the Office of Management and Budget’s (OMB) 2010 definition of metropolitan and nonmetropolitan counties. We further refine nonmetropolitan counties into those that are “adjacent” to a metropolitan county and those that are nonadjacent, or “remote” nonmetropolitan counties. Looking at the average number of both chain (Figure 2) and independent (Figure 3) pharmacies we can refine our understanding of the broad national patterns (Figure 1). To be able to compare counties across groupings that vary significantly by population, we compute the number of pharmacies per 1,000 persons.
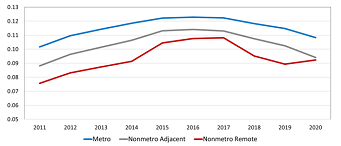
As noted above, the concentration of chain pharmacies is higher in metropolitan counties with the lowest concentration in nonmetropolitan remote counties (Figure 2). The growth in the concentration of chain pharmacies trends upward across all three types of counties until 2017 when there is a noticeable decline. This reflects the consolidation of even chain pharmacies into fewer and larger stores. Perhaps more important, it is in this period that on-line pharmacy services became more prevalent. Indeed, there is a movement amongst many health insurers to require patients to use specific online services to have long-term prescriptions filled, oftentimes dictated by the Pharmacy Benefit Manager (PBM). Further, while established drug chains like CVS and Walgreens have long offered mail delivery services for prescriptions, some big names like Amazon have more recently jumped intothe online pharmacy business. Other newcomers include GeniusRx, Honeybee Health, Ro Pharmacy, ScriptCo Pharmacy, and Mark Cuban’s Cost Plus Drug Co. They, along with more established online pharmacies likeCostco.com and HealthWarehouse.com, offer low-cost prescription drugs but they cannot offer the health care services of in-person pharmacists. The uptick in the concentration of chain pharmacies in nonmetropolitan remote counties from 2019 to 2020 breaks the pattern suggesting that the market in remote rural areas is changing.
The pattern for the concentration of independent pharmacies across the three-part rural-urban spectrum is much more stable than chain pharmacies (Figure 3). Here independent pharmacies, once population is accounted for, tend to be more likely to be present in remote rural areas and less likely to be in metropolitan areas. Also, the decline in chain pharmacies stores driven by the advent of on-line pharmacies, is not evident with independent pharmacies. Indeed, there is mild evidence of an increase in the concentration of independent pharmacies post 2017. This latter trend is particularly evident in rural remote counties. The impact of COVID on the concentration of independent pharmacies is clear for metropolitan and nonmetropolitan adjacent counties, but again remote rural counties are moving in the opposite direction.
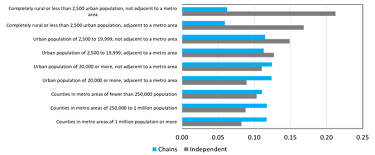
To further explore the differences between the presence of chain and independent pharmacies across the rural-urban spectrum we group counties by the classification that is widely referred to as the Beale Codes. This is a classification scheme that distinguishes metropolitan counties by the population size of their metro area, and nonmetropolitan counties by degree of urbanization and adjacency to a metro area. There are nine classifications ranging from counties with a central place of at least onemillion people to remote rural (nonadjacent) with no places with a population of no more than 2,500. Because the Beale Code uses the Office of Management and Budget’s definition of metropolitan areas, the most current classifications reflect the 2010 Census. Further, we calculated an annual average over the 2011 to 2020 period.
The pattern of chain pharmacies being more predominant in more urban (metro) areas while independent pharmacies are more predominant in rural areas is evident from the Beale Code bases comparisons (Figure 4). Indeed, most rural counties have no chain pharmacies present at any time over the 2011 to 2020 study period: those that are classified as completely rural or less than 2,500 urban population but are adjacent to a metro area, 99 out of 219 counties (45.2%) and for those that are classified as completely rural or less than 2,500 urban population and not adjacent to a metro area 240 out of 414 counties (58.0%) have no chain pharmacies. These same rural counties are much more dependent on independent pharmacies. Those completely rural but adjacent only 15.5% and 22.0% of the completely rural and non-adjacent have no independent pharmacies. Of the 633 counties that are classified in these “most rural” (Beale Code groups 8 and 9) 95 (15.0%) have no pharmacies of either type over the study period. This islargely consistent with the findings of Qato and her coauthors (2017).
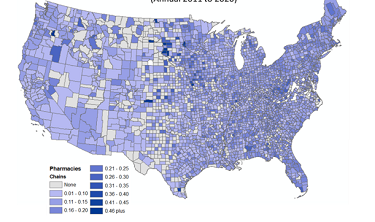
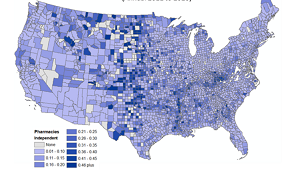
A mapping of the annual average number of chain pharmacies, again adjusted for population, reveals that counties without chain pharmacies are largely scattered across the U.S. but are most likely to be in the Great Plains, particularly from North Dakota south to western Texas (Map 1). From simple firm location theory (see Shaffer, Deller and Marcouiller 2004) it is likely that there is simply not a sufficient population base in many of these more rural counties to support a pharmacy, particularly a chain pharmacy. But a comparable mapping of independent pharmacies suggests that these rural counties in the Great Plains that are “chain pharmacy deserts” have relatively high concentrations of independent pharmacies (Map 2). While one must keep in mind that these are population-adjusted concentrations, it is clear that rural communities are particularly dependent on independent pharmacies.
The shock of COVID-19 was particularly hard on independent pharmacies and coincides with an increase in demand for the services they provide, namely vaccinations, Covid-19 testing, and providing personal protected equipment (PPE). Like many businesses that hinge on face-to-face interactions with customers, the sharp decline in non-prescription sales placed many independent pharmacies at risk of closure. Indeed, other than remote rural, there was a noticeable decline in the number of pharmacies between 2019 and 2020 (Figure 3). ). The future of independent pharmacies, particularly in rural communities, is increased competition from both chain and online pharmacies. Increasingly health insurers are requiring people to use designated pharmacies, often on-line and increasingly pharmacies owned and operated by the insurance companies themselves.
Rural independent pharmacies face several challenges beyond the competition from chain pharmacies, health insurance providers, and changes in Medicare Part D and other federal programs. One major challenge is the ability to attract pharmacists to not only locate in rural communities but to assume ownership of an independent pharmacy. Pharmacy students graduate with an average of $179,514 in student loan debt, according to the
American Association of Colleges of Pharmacy. This debt load affects the career choices recent grads make when entering the workforce. Survey work by DiDonato et.al. (2012) finds that the top four issues that new pharmacists consider in career choice are: (1) salary, (2) location, (3) benefits, (4) positive internship experience, and certainly these factors are not confined to those in pharmacy. Besier et.al. (1992) found that chain community pharmacies, which are more likely to be in metro areas, were chosen most frequently, and can offer a variety of choices on location, and offer higher salaries and benefits. This can make it hard to compete for pharmacies located in rural settings as observed by Traynor and Soresnsen (2005b):
“The challenges experienced by rural pharmacies in hiring staff and relief pharmacists result from many factors, including the rural pharmacy’s inability to offer competitive salaries and benefits…” (emphasis added)
Average salaries for pharmacists lag behind in rural areas versus those in urban settings (Figure 6). The average annual compensation for a pharmacist in a remote rural (nonmetro nonadjacent) county is $126,267 or $10,522 per month. For the average pharmacy graduate that means nearly 20% of monthly before tax income is going to student debt repayment for those working in rural areas. For a metro county, where the average salary is $148,8862 annually, or $12,405 per month, the percent ofincome to student debt drops to 16.3%. No wonder income rises to the top of employment considerations.
These high levels of student debt are a deterrent to business ownership as well. In “Indebted and Drained” Deller and Parr (Choices, 2020) note that student loan debt can prevent would-be entrepreneurs from accessing capital for starting a business and mentally inhibit them from wanting to take on more debt or risk. Thus, the highlevels of student debt incurred by pharmacy students also create barriers to financing the ownership of rural pharmacies. As increasing shares of ever-growing costs of a pharmacist degree are placed on students, the negative impact of this student debt will increasingly make the selection of being a rural independent pharmacist less likely.
There are some strategies, however, that might help address the shortfall of rural pharmacists. For example, developing and strengthening a network of rural independent pharmacies to provide internship programs for pharmacy students would encourage students to consider rural areas. As indicated in the career choice survey by DiDonato and her colleagues (2012), having a positive internship experience can encourage students to pursue careers in that type of pharmacy work. Further, Traynor and Soresnsen (2005a) suggest that ownership of a rural pharmacy is of interest if the students come from a more rural background. Further, increasing opportunities to work in community pharmacies can keep student interest, Sweaney, et.al. (2014) find that pharmacy students are interested in the idea of ownership, but if it is not part of the training program that interest drops off. Like programs and incentives aimed at attracting physicians to rural communities, these strategies could be used to attract and retain pharmacists to rural areas. Because students from rural areas are more likely to express interest in working in pharmacies in rural areas, recruitment, and scholarships for students in rural areas to pursue degrees in pharmacy could increase these numbers.
Some pharmacy school graduates may be eligible for student loan forgiveness through the Public Service Loan Forgiveness Program (PSLF), as well as programs through the National Institute of Health. Only a few states offer loan student forgiveness for pharmacists who work in rural and other underserved areas. Expanding student loan
forgiveness programs may incentivize new pharmacists to consider or revisit the idea of working at or owning an independent community pharmacy. Alternatively, some rural communities have recruited medical doctors by agreeing to pay a certain amount of the doctor’s student debt if they establish a practice within the community for a minimum number of years. A similar approach could be applied to pharmacists.
There is also the additional challenge of not only attracting pharmacists to rural communities but also expanding their interest in operating an independent pharmacy. As is the case in many professions from accounting to farming, business owners must have the knowledge and skills in their profession as well as be proficient in running a business. Business development skills like bookkeeping, recordkeeping, taxes, marketing, and personnel management geared toward pharmacies, can provide pharmacists with the entrepreneurship skills necessary to own and operate a successful business. Exposure to being the owner of the pharmacy can be part of the internship programs described above and made part of their training program. These types of strategies can only expose the pharmacy student to the idea of being the owner of the pharmacy and will not adequately prepare them to actually operate the business. Here communitiesmust provide technical assistance as they might any other business within the community whether that assistance is through local, regional, or even state resources.
Like in other types of business, succession planningserves to ensure that vital businesses remain in the community. Pharmacists are well networked and have robust alumni programs. Offering mentorships and internships for students and business succession planning to alumni could foster interest in pharmacy ownership. Traynor and Soresen (2005b) found that 26% of rural pharmacy owners in Minnesota were interested in selling within three years and 62% within ten years. This presents an opportunity to pair those interested in community pharmacy with those established pharmacies interested in selling. A study by Ayres, Leistriz, and Stone (1992) found that rural communities that had active programs that helped existing business owners transition their business to new owners kept the businesses active in the community. This could be the transition to the pharmacist being owner operator or even another community entrepreneur to jointly own and operate the pharmacy in partnership with a pharmacist.
The National State-Based Pharmacy Workplace survey by Schommer et.al. (2022) found that job satisfaction among pharmacists and pharmacy personnel was at its lowest point in 20 years, while job stress was at an all-time high for those in community pharmacy settings. This is especially true for pharmacists working in independent pharmacies who do not have other staff available to relieve them for time off. Traynor and Sorensen (2005b) found that the lack of relief.
pharmacists increases stress and frustration of rural independent pharmacists. As noted by Casey et.al. (2002) developing a network of “relief pharmacists” that can step in and allow the primary pharmacist vacation time mayimprove job satisfaction, alleviate burnout, and avoid medication errors. The proposed network of rural independent pharmacies aimed at providing internship opportunities could also provide a network of “relief pharmacists” as well as technical support services for pharmacists wishing to become owners of the pharmacy.
One option that some rural independent pharmacies have pursued is the integration with larger entities such as hospitals and insurance companies. Such integration can decrease overhead costs for independent pharmacies and ease the burden of reimbursement and recordkeeping. Integration also encourages the shift to patient-focused care (Schommer, et.al. 2022). As rural hospitals consolidate with larger health care systems, horizontal integration can decrease operating costs for the pharmacist and improve health outcomes for patients. Luder et.al (2015) found that when hospitals coordinated care with community pharmacies, patients had fewer hospital readmissions.
Other options that could help rural independent pharmacies require policy changes that are beyond the control of local communities and pharmacy schools. The implementation of Medicare Part D in 2006 expanded prescription coverage to Medicare recipients but came with low reimbursement rates for pharmacies, particularlyindependent community pharmacies who relied on sales of prescriptions by patients paying cash more than retail chain pharmacies. As noted by Klesper, et.al. (2010: p174):
“…Medicare Part D had an unintended effect on patient access to community pharmacy services. In particular, it was related to a decrease in the number of independent pharmacies and increased rate of closure of pharmacies that were the sole provider in their community.”
Unintended or not, this policy change left many rural residents without access to a pharmacy. Changes to reimbursement rates for Medicare Part D prescriptions, as well as allowing reimbursement for patient counseling (Pharmacists are not currently recognized as health care providers under Medicare) can make it more cost-effective to operate a pharmacy.
Also worth exploring is the predominance of Pharmacy Benefit Managers in the marketplace for prescriptions. PBMs negotiate drug prices with manufacturers and act as a third-party agents for health insurance plans. The increasing vertical integration of PBMs has led to three firms owning over 80% of the market (Bai, et.al. 2018). The United States is one of the only industrialized countries that rely on market forces, instead of government price control methods, to determine drug prices (So-Yeon, et.al. 2020). Independently owned pharmacies may be disproportionately affected by the surge of PBMs as these agents often guide patients away from using these pharmacies, even when they are more convenient for patients.
Another option that has been explored is the use of telehealth type models to bridge the gap and perhaps even be a method for providing “relief pharmacists” as discussed above. With telehealth, a pharmacist in a central location can work with local pharmacy technicians to interface with clients. After consultation with the pharmacist remotely, the pharmacy technician can then distribute the prescriptions to the client. In many states, however, regulations require that the actual handling of the prescription with the client must be done in person with a pharmacist. One approach would be to elevate the training requirements of key pharmacy technicians and rely on the centrally located pharmacist to ensure quality of services. This, however, would require changes in state law which may be difficult.
Access to health care in rural communities has been the focal point of discussion for a number of years. Much of the discussion has focused on rural hospitals with little attention to pharmacies. Access to the services offered by pharmacies is a vital piece of the complex milieu of health care service delivery. For rural communities, the historical dependency on independently owned and operated pharmacies has placed rural residents at risk of losing access to the key services offered by pharmacies. As chain pharmacies, including on-line companies, have expanded there has been a noticeable decline in the number of independent pharmacies. The data suggests that COVID-19 related economic impacts have been particularly difficult for these independent pharmacies upon which so many rural communities depend. Unfortunately, lower salaries offered to rural pharmacists coupled with ever-increasing student debt, makes locating in rural communities unattractive to most recently graduated pharmacists. While there are some strategies that some rural communities are pursuing to retain their independent pharmacies, there may need to be more substantial policy changes at the federal and state level to address the growing rural pharmacy crisis.
Adynski, Gillian I., and Leah L. Morgan. (2021). "A Systematic Review of the Strategies to Address Health Worker Shortage in Rural and Remote Areas of Low-and Middle-Income Countries." Online Journal of Rural Nursing & Health Care 21(2).
Ayres, J., L. Leistritz, and K. Stone. (1992). "Rural Retail Business Survival: Implications for Community Developers." Community Development 23(2): 11-21.
Bai G., A.P. Sen, and G.G. Anderson. (2018). “Pharmacy Benefit Managers, Brand-Name Drug Prices, and Patient Cost Sharing.” Annals of Internal Medicine 168(6):436–37
Besier J.L., and R. Jang. (1992). “Factors Affecting Practice-Area Choices by Pharmacy Students in the Midwest. American Journal of Hospital Pharmacy. 49: 598-602.
Casey, M.M., J. Klingner, and I. Moscovice. (2002). "Pharmacy Services in Rural Areas: Is the Problem Geographic Access or Financial Access?" The Journal of Rural Health 18(3): 467-477.
Deller, S.C. and J. Parr. (2020). “Indebted and Drained: Student Loans and Rural America.” Choices: The Magazine of Food, Farm and Resource Issues. 35(1).
DiDonato, K.L., K.A. Casper, J.L. Rodis, T.R. Green, and K.A. Kelley. (2012). "Assessment of Factors Influencing Recent Graduates' Selection of a Community Pharmacy Practice Site as Their First Practice Position." Currents in Pharmacy Teaching and Learning 4(2): 84-91.
Hawryluk, M. (2021). “Rural Americans in Pharmacy Deserts Hurting for Covid Vaccines.” Kaiser Health News. March 3. https://khn.org/news/article/last-drugstore-how-rural-communities-lose-independent-pharmacies/ (accessed June 17, 2022)
Kaufman, B.G., S.R. Thomas, R.K. Randolph, J.R. Perry, K.W. Thompson, G.M. Holmes, and G.H. Pink. (2016). "The Rising Rate of Rural Hospital Closures." The Journal of Rural Health 32(1): 35-43.
Kissi, M., J.D. Walston, and M.A. Badar. (2021). "Statistical Analysis of Rural Hospital Closures in the U.S.A." International Journal of Forensic Engineering and Management 1(2): 209-224.
Klepser, D.G., L. Xu, F. Ullrich, and K.J. Mueller. (2011). "Trends in Community Pharmacy Counts and Closures Before and After the Implementation of Medicare Part D." The Journal of Rural Health 27(2): 168-175.
Luder H.R., S.M. Frede, J.A. Kirby, K. Epplen, T. Cavanaugh, J.E. Martin-Boone, W.F. Conrad, D. Kuhlmann, and P.C. Heaton. (2015). “TransitionRx: Impact of Community Pharmacy Postdischarge Medication Therapy Management on Hospital Readmission Rate.” Journal of the American Pharmacists Association 355(3): 246-254.
Pednekar, P., and A. Peterson. (2018). “Mapping Pharmacy Deserts and Determining Accessibility to Community Pharmacy Services for Elderly Enrolled in a State Pharmaceutical Assistance Program.” PloS one 13(6): e0198173.
Qato, D.M., S. Zenk, J. Wilder, R. Harrington, D. Gaskin, and G.C. Alexander. (2017). "The Availability of Pharmacies in the United States: 2007–2015." PloS one 12(8): e0183172.
Salako, A., F. Ullrich, and K.J. Mueller. (2018). “Update: Independently Owned Pharmacy Closures in Rural America, 2003-2018.” Brief No. 2018-2 Center for Rural Health Policy Analysis, Rural Policy Research Institute, University of Iowa.
Scheidt, L., A. Heyen, and T. Greever-Rice. (2021). "Show Me the Nursing Shortage: Location Matters in Missouri Nursing Shortage." Journal of Nursing Regulation 12(1): 52-59.
Schommer, J.C., S. Lee, C.A. Gaither, N.A. Alvarez, and A.M. Shaughnessy. (2022). "Improving the Experience of Providing Care in Community-Based Pharmacies." Pharmacy 10(4): 67.
Shaffer, R., S.C. Deller, and D.W. Marcouiller. (2004). Community Economics: Linking Theory and Practice. No. Ed. 2. Blackwell Publishing.
So-Yeon, K., G. Bai, M.J. Di Stefano, M.P. Socal, F. Yehia, G.F. Anderson. (2020) “Comparative Approaches to Drug Pricing.” Annual Review of Public Health 41(1): 499-512
Stratton, T.P. (2001). "The Economic Realities of Rural Pharmacy Practice: The Economics of Rural Health." The Journal of Rural Health 17(2): 77-81.
Straub, L.A., and S.A. Straub. (1999). "Consumer and Provider Evaluation of Rural Pharmacy Services." The Journal of Rural Health 15(4): 403-412.
Sweaney, A.M., K.A. Casper, C.D. Hoyt, and A.M. Wehr. (2014). "Student Pharmacists' and Recent Graduates' Perception of and Interest in Independent Pharmacy Ownership." Innovations in Pharmacy 5(4): 1-10.
Traynor, A.P., and T.D. Sorensen. (2005a). "Student Pharmacist Perspectives of Rural Pharmacy Practice." Journal of the American Pharmacists Association 45(6): 694-699.
Traynor, A.P., and T.D. Sorensen. (2005b). "Assessing Risk for Loss of Rural Pharmacy Services in Minnesota." Journal of the American Pharmacists Association 45(6): 684-693.