
This article is based on collaborations developed through the Northeast Center for Rural Development small grant Best Practices in Bike/Pedestrian Trail Data and Monitoring.

Social distancing measures are changing how we think about and use outdoor spaces. Since the start of the COVID-19 pandemic and associated restrictions on many events and activities, use of trails in communities across the United States has surged, in some areas up to 200%. As the pandemic continues, park managers remain focused on urgent public health and safety concerns. However, immediate and longer term increased outdoor space use poses both challenges and opportunities for trail and environmental management, public health, economic asset development, equity and access. It is yet to be seen if these short-term reactive trends will lead to long-term changes either in recreational behavior or community recreation policy. Meanwhile, exploring ongoing impacts may help communities identify potentially beneficial strategies, policies, and programs. As of this writing, policies continue to shift to address the changing nature of the pandemic from region to region, and from local to national levels. Our objective is to explore these potential implications from the perspective of two stakeholder groups associated with recreation use of outdoor space: trail managers and trail users.
A growing number of studies and reports document a surge in trail use during the COVID-19 pandemic, primarily provided by data collected through monitoring programs, trail manager, and user surveys (Bradley et al., 2020; Derks et al., 2020; Oftedal, 2020; Pennsylvania Environmental Council, 2020; Kapp and Oberg, 2020). Typically, these data are collected through existing installed data counters, TrafX or Eco-counters, from which data from previous years provide an annual baseline for comparison. For example, a study of ten Minnesota trails found that nine of the ten monitored locations set daily traffic records in the year 2020 for March and April trail use, and that trail use increased further with every successively introduced pandemic-related restrictive measure (Oftedal, 2020). In the northeast, the Pennsylvania Environmental Council reported individual trail increases of 100-200% for some trails, and an overall increase in use of 52% in March across all trails compared to 2019, effectively kicking off the use season a month early (Pennsylvania Environmental Council, 2020).
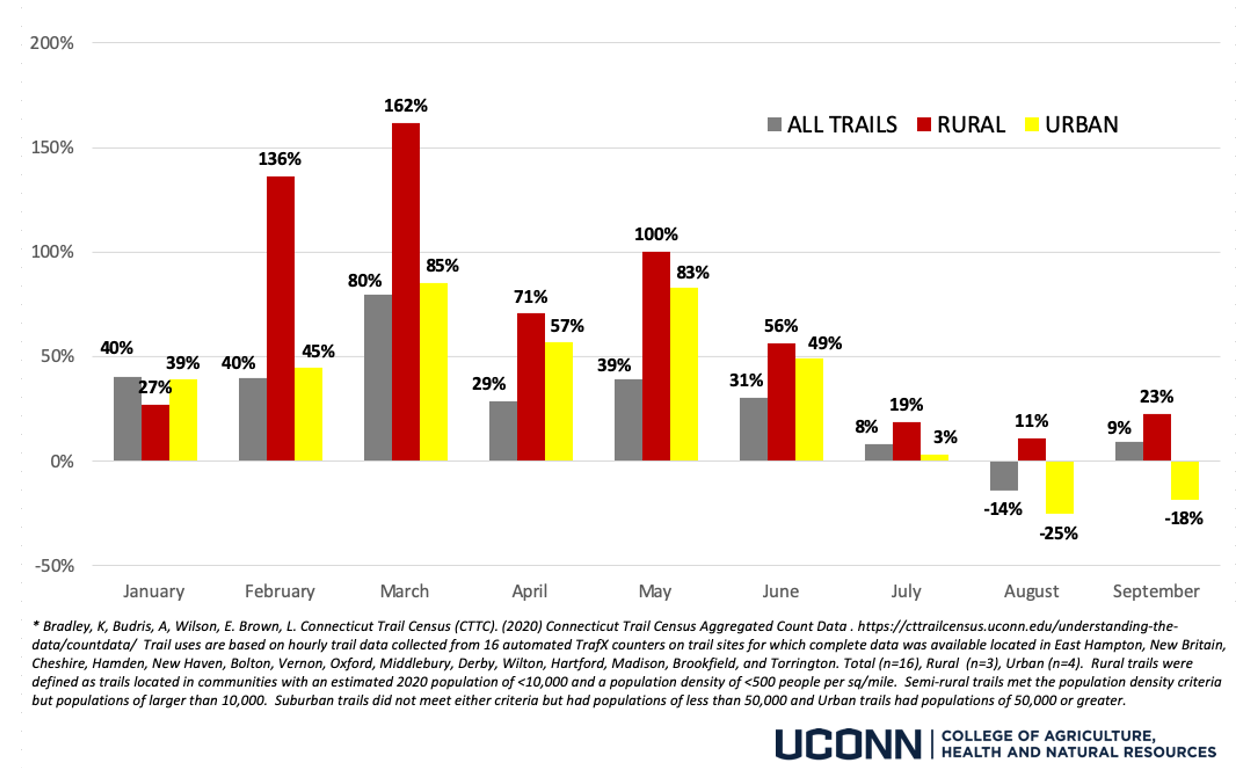
Similarly, the Connecticut Trail Census, when compared to 2019 data, documented monthly use increases through July 2020; the greatest change occurring in the month of March (82%). However, further analysis comparing 2019 and 2020 data from the Connecticut Trails Census revealed that these patterns were not consistent across all types of trails. For example, analysis of subset of sixteen trails including three in rural areas1 found that rural trails experienced an increase in use in 2020 over 2019 during every month of the year, peaking at a 162% increase in March 2020. In contrast, trail use on semi-rural, suburban, and urban trails in August 2020 dropped from 2019 numbers. Yet, rural trail use in 2020 was still greater than 2019 by more than 11% (Bradley et al., 2020).
Why is trail use increasing? This surge may be the result of both displacement from other routine activities, displaced use from areas like parks that may have closed, and increased interest among new users. Since the start of the pandemic, the National Parks and Recreation Association has conducted bi-weekly “snapshot” surveys of amenity managers regarding recreational amenities that were open, partly open, or closed due to social distancing measures. During peak closures in spring 2020 when more than 50% of sports facilities and playgrounds were closed, over 90% of trails were either open or partly open -- although percentages varied from region to region nationally. As a whole, trails and local or neighborhood parks have been the most universally open outdoor recreational resources throughout the course of the pandemic (National Recreation and Park Association, 2020).
But this does not tell the whole story. Recent data from a survey of the Leave No Trace network suggests changes in outdoor recreation use among enthusiasts, defined as those who are highly reliant on outdoor recreation as a means of leisure (Rice et al., 2020). Given stay at home orders, frequency of outdoor recreation among enthusiasts decreased from 5.07 days per week to 4.76 days per week (by 0.03 days for rural residents, 0.37 days for urban cluster1 residents and 0.52 days for urban residents), average distance traveled decreased from 3.5 miles to 1.94 miles, average group size decreased from 5.61 to 1.85 persons (Rice et al., 2020). While these data are important for understanding the immediate impacts of closures on enthusiast users, it is important to note that data were collected early in the pandemic (April 2020) when many areas we discouraging any trips outside the home and so may not reflect long term trends. We suspect, however, that “new” users are comprising a larger proportion of all trail users during the pandemic, and existing users are participating in trail use more frequently overall. Both posits are anecdotally supported by preliminary Connecticut Trails Census data (n = 993), which suggest that about 16% of respondents did not use the trails prior to the COVID-19 pandemic, whereas 22% of existing users use trails more frequently (Brown and Bradley, 2020).
The possibility that more rural people are engaging in physical activity on trails may be a positive sign for public health in rural communities affected by COVID-19. Several studies have found positive relationships between presence of trails and physical activity as well as trail use and physical activity (Frost et al., 2010; Brownson et al., 2004). Additionally, throughout the COVID-19 pandemic, public health experts have advocated for increased accessibility and availability of greenspaces to promote socially distant physical activity (Slater et al., 2020). The physical and mental health benefits of activity in greenspaces is well documented, and suggests that even a limited time engagement in exercise in greenspaces may be associated with lower rates of heart disease, depression, and stroke; lower blood pressure, enhanced immune system function, and greater self-esteem and mood than in individuals who do not pursue such activity (Barton and Pretty, 2010; Coon et al., 2011; Gladwell et al., 2013; Harvard Medical School, 2009; Kuo, 2011; Li et al., 2011; Li et al., 2008; Park et al., 2007; Wood et al., 2016).
However, the potential for rural communities and vulnerable populations to achieve gains in health outcomes through use of trails and greenspaces depends in part on their ability to overcome barriers to physical activity. These barriers may include factors related to access, socioeconomics, available time for recreation, and individual motivation (Gavarkovs et al., 2017; Kurti et al., 2015), all factors that may also be affected by job losses, school closures, and other stressors related to the pandemic.
Many rural areas face additional vulnerabilities that place populations at greater risk for COVID-19 including a greater proportion of the population comprised of relatively older, uninsured, and people with existing health conditions; fewer physicians, unavailability of mental health services, and greater proportion of the population with a disability (Peters, 2020). Eighty percent (80%) of deaths attributed to COVID-19 have been among adults aged 60 years or older (Centers for Disease Control Morbidity and Mortality Weekly Report, 2020). These observations raise serious public health concerns, considering that 19.3% of the U.S. population resides in rural areas, and the average age of rural Americans being 73.3 years old (Wong et. al., 2019). Risk for obesity is also greater among rural populations, such that the odds of being obese among rural adults is 1.19 times greater than that among urban adults (Trivedi et al., 2015). Chronic comorbidities, including obesity, hypertension, diabetes, cardiovascular disease, cerebrovascular disease, respiratory disease, kidney disease, and malignancy are clinical risk factors for a severe or fatal outcome associated with COVID-19, with obesity being the most prevalent and respiratory disease being the most strongly predictive (Zhou et al., 2020).
People living alone have also faced particular risks of isolation and loneliness during the pandemic; related to this, older adults in rural areas are among the most likely to be isolated from creative, technologically-based adaptations to social activities (Henning-Smith, 2020). Therefore, characteristics of individuals most at risk of developing severe cases of COVID-19 are similar to those who have reported greater frequency of social isolation - older adults and people with underlying medical conditions (Lewis et al., 2020).
Even for those who have not experienced the COVID-19 illness, public health effects of the pandemic and associated impacts of social distancing guidelines will likely be observed in communities for many years to come. Long-term isolation could expedite cases of post-traumatic stress (Brooks et al., 2020) and exacerbate existing unfavorable health conditions (Ortiz-Ospina, 2019 as cited in Samuelsson et al., 2020).
The introduction of significant numbers of new users on rural trails presents opportunities and challenges for management. Even with decreased staffing and volunteers, rural trail managers have been forced to adapt quickly with public health signage and guidelines and changing maintenance schedules or facility structures to address littering, crowding, and overuse (Kapp and Oberg, 2020; Pennsylvania Environmental Council, 2020). When asked to identify positive and negative impacts of the COVID-19 pandemic on trails, 97 trail managers in Connecticut identified parking lot capacity limitations and crowding, littering, increased number of users, changes in standard maintenance (bathrooms, trash collection, mowing, etc.), conflict among trail users, change in use patterns, and change in user demographics among the top negative impacts (Brown and Bradley, 2020).
Response by recreation managers to these factors has included in some cases, trail and area closures, but more often the increased promotion of lesser used trails, improved signage, and facility changes such as making overflow parking available.
If trail use continues to remain greater than pre-pandemic levels, land use managers may consider adding trails to existing networks or increasing the quantity of accessible greenspaces to reduce user density. From a policy perspective, this may have implications for funding and resource needs to support increased use and mitigate impacts of overuse. Other changes to trails or green spaces may include improved or increased outdoor programming, spatial design that supports social distancing, or overall improvements in greenspace infrastructure. The COVID-19 crisis also presents the potential for better integration of health into greenspace planning and design.
While current discussions are largely around disease control (Honey-Roses et al., 2020), the pandemic offers a new lens for understanding who has access to safe outdoor spaces like trails and parks, and in particular, how systemic inequalities affect the accessibility of greenspace amenities to Black, Indigenous, people of color, and low-income communities.
This is particularly relevant if a significant number of new users are from urban areas that otherwise lack greenspace access, only have proximate access to greenspaces that may be closed during the pandemic, or perceive heavily used urban greenspaces to be unsafe during the pandemic. While the short term data of trail enthusiasts cited earlier found distance traveled to have decreased during the lockdown period of the pandemic, anecdotal analysis of data collected by the Connecticut Trail Census in 2020 suggests that new users during the pandemic may be traveling further from home to use greenspaces that users in previous years; (87%) of new trail users reported living outside the zip code where the trail was located while 69% of trail users overall reported as using trails outside their home zip code.
In some urban areas, many parks and greenspaces with playgrounds, play structures or other features that posed transmission and safety hazards were restricted or closed during the pandemic, raising the possibility that urban residents might have had less access to these spaces. Disparity in access to greenspaces between urban and rural populations is well documented, and in some cases may be traced to discriminatory policy measures such as exclusionary zoning and disparities in funding that disadvantaged people of color. As an example, a review of these disparities in Denver found the geographic location of greenspace amenities largely followed the historic delineations of discriminatory red-lining whereby residents of some neighborhoods were systematically denied access to financial resources (Forrest, 2018; Campbell, 2019; Moore, 2019; Rigolon and Németh, 2018). More resources on equity and access in greenspaces may be found in the Guide to Anti-Racism in the Outdoors (Brown & Rakow, 2020).
COVID-19 presented many social challenges, but the pandemic also offers opportunities for rural land use managers and planners to improve access to trails and greenspaces while maintaining environmental standards, and thereby improve the health of rural populations. The increased interest and awareness serves as a call to better understand needs for expanding existing trail systems, as well as the need for connectedness of trails to existing and potential users. This will involve thoughtful, regional efforts to address land use involving a wide variety of partners. There is opportunity for trail managers and planners to continue current trends through collaborations with public health officials to support and expand outdoor recreational amenities that are safe, accessible, and address current inequities that inhibit use by Black, Indigenous, or people of color.
We believe land use and trail managers must actively address environmental justice issues to address inequitable access and create safe recreational environments for all users and that these efforts must be bolstered with resources and funding. Ensuring that trail and greenspace facilities remain accessible is essential. When access to natural environments such as trails and parks is limited, individuals are less likely to reap the physical and mental health benefits (Rung et al., 2011; Samuelsson et al., 2020; Rice et al., 2020). Land use and greenspace managers, trail advocates, and resource providers should take a leadership role in understanding and providing education about systemic environmental injustices, amplifying voices of Black, Indigenous, and people of color; and ensuring diverse representation on boards and land use decision making committees (Discher, 2020). We hope this work will spur investment in greenspace resources to support increased use as well as the development of more applied and interdisciplinary research to inform better regional land use planning and community development.
Barton, J., and J. Pretty. 2010. “What is the Best Dose of Nature and Green Exercise for Improving Mental Health? A Multi-Study Analysis.” Environmental Science and Technology, 44(10), 3947–3955.
Bradley, K, A. Budris, E. Wilson, and L. Brown. 2020. “Connecticut Trail Census Aggregated Count Data.” Connecticut Trail Census. University of Connecticut. Available online: https://cttrailcensus.uconn.edu/understanding-the-data/countdata/.
Brooks, S.K., R.K. Webster, L.E. Smith, L. Woodland, S. Wessely, N. Greenberg, and G.J. Rubin. 2020. “The psychological impact of quarantine and how to reduce it: Rapid review of the evidence.” The Lancet, 395(10227), 912–920.
Brown, L. and K. Bradley. 2020. “Impacts of COVID-19 Trail Manager Survey Analysis.” Unpublished. Connecticut Trail Census. University of Connecticut.
Brown, L. and K. Bradley. 2020. “2020 Connecticut Trail Census Aggregated Survey Data Analysis.” Unpublished. Connecticut Trail Census. University of Connecticut.
Brown, L. and D. Rakow. (2020). Antiracism in the Outdoors. https://s.uconn.edu/antiracismoutdoors.
Brownson, R.C., E.A. Baker, R.L. Boyd, N.M. Caito, K. Duggan, R.A. Housemann, M.W. Kreuter, T. Mitchell, F. Motton, C. Pulley, T.L. Schmid, and D. Walton. 2004. “A community-based approach to promoting walking in rural areas.” American Journal of Preventive Medicine, 27(1), 28–34.
Campbell, A.F. 2016, September 29. “Inequality in American Public Parks.” The Atlantic. Available online: https://www.theatlantic.com/business/archive/2016/09/inequality-in-american-public-parks/502238/.
Centers for Disease Control Morbidity and Mortality Weekly Report. 2020. “Severe Outcomes Among Patients with Coronavirus Disease 2019 (COVID-19)—United States, February 12–March 16, 2020.” Morbidity and Mortality Weekly Report, 69.
Derks, J., L. Giessen, and G. Winkel. 2020. “COVID-19-induced visitor boom reveals the importance of forests as critical infrastructure.” Forest Policy and Economics, Volume 118.
Discher, J. 2020, November. “Environmental Injustice Leads to a Disproportionate Number of COVID-19 Cases in Black Ohioans.” The Ohio Environmental Council. Available online: https://theoec.org/wp-content/uploads/2020/11/2020-Ohio-Public-Interest-Environmental-Justice-Writing-Competition-1.pdf#page=15.
Forrest, S. 2018, August 31. “Study: Denver’s inequities in park access traced to segregation, funding policies.” University of Illinois. Available online: https://news.illinois.edu/view/6367/689109.
Frost, S.S., R.T. Goins, R.H. Hunter, S.P. Hooker, L.L. Bryant, J. Kruger, and D. Pluto. 2010. “Effects of the Built Environment on Physical Activity of Adults Living in Rural Settings.” American Journal of Health Promotion, 24(4), 267–283.
Gavarkovs, A.G., S.M. Burke, and R.J. Petrella. 2017. “The Physical Activity-Related Barriers and Facilitators Perceived by Men Living in Rural Communities.” American Journal of Men’s Health, 11(4), 1130–1132.
Gladwell, V.F., D.K. Brown, C. Wood, G.R. Sandercock, and J.L. Barton. 2013. “The great outdoors: How a green exercise environment can benefit all.” Extreme Physiology and Medicine, 2(1), 3.
Harvard Medical School. 2009. “Walking: your steps to health.” Harvard Medical School, para 1-12. Available online: http://www.health.harvard.edu/newsletter_article/Walking-Your-steps-to-health.
Henning-Smith, C. 2020. “The Unique Impact of COVID-19 on Older Adults in Rural Areas.” Journal of Aging and Social Policy, 32:4-5, 396-402.
Honey-Rosés, J., I. Anguelovski, V.K. Chireh, C. Daher, C.K. Bosch. J.S. van den Litt, V. Mawani, M.K. McCall, A. Orellana, E. Oscilowicz, U. Sánchez, M. Senbel, X. Tan, E. Villagomez, O. Zapata, and M.J. Nieuwenhuijsen. 2020. “The impact of COVID-19 on public space: An early review of the emerging questions – design, perceptions and inequities.” Cities and Health, 0(0), 1–17.
Kapp, A and E. Oberg. 2020. “Taking Care of Our Trails and Parks in the Midst of COVID-19.” Rails-to-Trails Conservancy. [Blog post]. Available online: http://www.railstotrails.org/trailblog/2020/may/22/taking-care-of-our-trails-and-parks-in-the-midst-of-covid-19/.
Kuo, F.E. 2011. “Parks and Other Green Environments: Essential Components of a Healthy Human Habitat.” Australasian Parks and Leisure, 14(1), 10.
Kurti, A.N., H. Logan, T. Manini, and J. Dallery. 2015. “Physical activity behavior, barriers to activity, and opinions about a smartphone-based physical activity intervention among rural residents.” Telemedicine Journal and E-Health, 21(1), 16–23.
Lewis, C., T. Shah, G. Jacobson, A. McIntosh, and M.K. Abrams. 2020. “How the COVID-19 pandemic could increase social isolation, and how providers and policymakers can keep us connected.” The Commonwealth Institute. Available online: https://www.commonwealthfund.org/blog/2020/how-covid-19-pandemic-could-increase-social-isolation-and-how-providers-and-policymakers.
Li, Q., K. Morimoto, M. Kobayashi, H. Inagaki, M. Katsumata, Y. Hirata, K. Hirata, H. Suzuki, Y.J. Li, Y. Wakayama, T. Kawada, B.J. Park, T. Ohira, N. Matsui, T. Kagawa, Y. Miyazaki, and A.M. Krensky. 2008. “Visiting a forest, but not a city, increases human natural killer activity and expression of anti-cancer proteins.” International Journal of Immunopathology and Pharmacology, 21(1), 117–127.
Li, Q., T. Otsuka, M. Kobayashi, Y. Wakayama, H. Inagaki, M. Katsumata, Y. Hirata, Y. Li, K. Hirata, T. Shimizu, H. Suzuki, T. Kawada, and T. Kagawa. 2011. “Acute effects of walking in forest environments on cardiovascular and metabolic parameters.” European Journal of Applied Physiology, 111(11), 2845–2853.
Moore, S. 2019, August 9. “Park Inequities Are Symptoms of a Bigger Problem.” Healthy Places by Design. Available online: https://healthyplacesbydesign.org/park-inequities-are-symptoms-of-a-bigger-problem/.
National Recreation and Park Association. 2020, November 12. “Parks Snapshots Surveys.” Available online: https://www.nrpa.org/publications-research/parks-snapshot-surveys/.
Oftedal, A. 2020, April 27. “Trail use has surged in response to the COVID-19 pandemic – Parks and Trails Council of Minnesota.” [Blog post]. Available online: https://www.parksandtrails.org/2020/04/27/trail-use-covid19/.
Park, B.J., Y. Tsunetsugu, T. Kasetani, T. Kagawa, and Y. Miyazaki. 2010. “The physiological effects of Shinrin-yoku (taking in the forest atmosphere or forest bathing): Evidence from field experiments in 24 forests across Japan.” Environmental Health and Preventive Medicine, 15(1), 18–26.
Pennsylvania Environmental Council. 2020, June 8. “Measuring COVID-19’s Impact on PA Trail Use.” [Blog post]. Available online: https://pecpa.org/pec-blog/measuring-covid-19s-impact-on-trail-use/.
Peters, D.J. 2020. “Community Susceptibility and Resiliency to COVID‐19 Across the Rural‐Urban Continuum in the United States.” The Journal of Rural Health, 36(3), 446–456.
Rice, W.L., T.J. Mateer, N. Reigner, P. Newman B. Lawhon, and B.D. Taff. 2020. “Changes in recreational behaviors of outdoor enthusiasts during the COVID-19 pandemic: Analysis across urban and rural communities.” Journal of Urban Ecology, 6(1).
Rigolon, A., and J. Németh. 2018. “What Shapes Uneven Access to Urban Amenities? Thick Injustice and the Legacy of Racial Discrimination in Denver’s Parks.” Journal of Planning Education and Research. Available online: https://doi.org/10.1177/0739456X18789251.
Rung, A.L., A.J. Mowen, S.T. Broyles, and J. Gustat. 2011. “The role of park conditions and features on park visitation and physical activity.” Journal of Physical Activity and Health, 8 Suppl 2, S178-187.
Samuelsson, K., S. Barthel, J. Colding, G. Macassa, and M. Giusti. 2020. “Urban nature as a source of resilience during social distancing amidst the coronavirus pandemic.” Center for Open Science PrePrints. Available online: https://doi.org/10.31219/osf.io/3wx5a.
Trivedi, T., J. Liu, J. Probst, A. Merchant, S. Jhones, and A.B. Martin. 2015. “Obesity and obesity-related behaviors among rural and urban adults in the USA.” Rural Remote Health, 15(4), 3267.
Wong, H., K. Moore, K.B. Angstman, and G.M. Garrison. 2019. “Impact of rural address and distance from clinic on depression outcomes within a primary care medical home practice.” BioMed Central Family Practice, 20(1), 123.
Wood, L., P. Hooper, S. Foster, and F. Bull. 2017. “Public green spaces and positive mental health – investigating the relationship between access, quantity and types of parks and mental wellbeing.” Health and Place, 48, 63–71.
Zhou, Y., Q. Yang, J. Chi, B. Dong, W. Lv, L. Shen, and Y. Wang. 2020. “Comorbidities and the risk of severe or fatal outcomes associated with coronavirus disease 2019: A systematic review and meta-analysis.” International Journal of Infectious Diseases, 99, 47–56.
1 In this study reported type of community of residence was adapted from the U.S. Census Bureau (2010): under 5,000, between 5,000 and 50,000, and over 50,000 residents